Women’s Cancer Communication Project
Coordinated by the European Institute of Women’s Health
Information on Cervical Cancer
 |
Cervical cancer is one of the most common cancers in women and occurs at the cervix, the opening to the uterus which is also called the womb. The highest incidence of cervical cancer occurs in women aged 40-55. In 2018, 315.000 women died worldwide of cervical cancer. |
It is estimated that 1 in 100 women will develop cervical cancer. The Human papillomavirus (HPV) is a common sexually transmitted virus and there are about 100 different known types.
Two types (16 &18) cause about 70% of cervical cancer or its prior development stage. Smear tests can identify the HPV virus and early treatment can prevent the development of cervical cancer cells.
Nearly 70% of women who die from cervical cancer have not had a routine smear test. Most cervical cancer cases can be successfully prevented if detected early enough through regular smear tests.
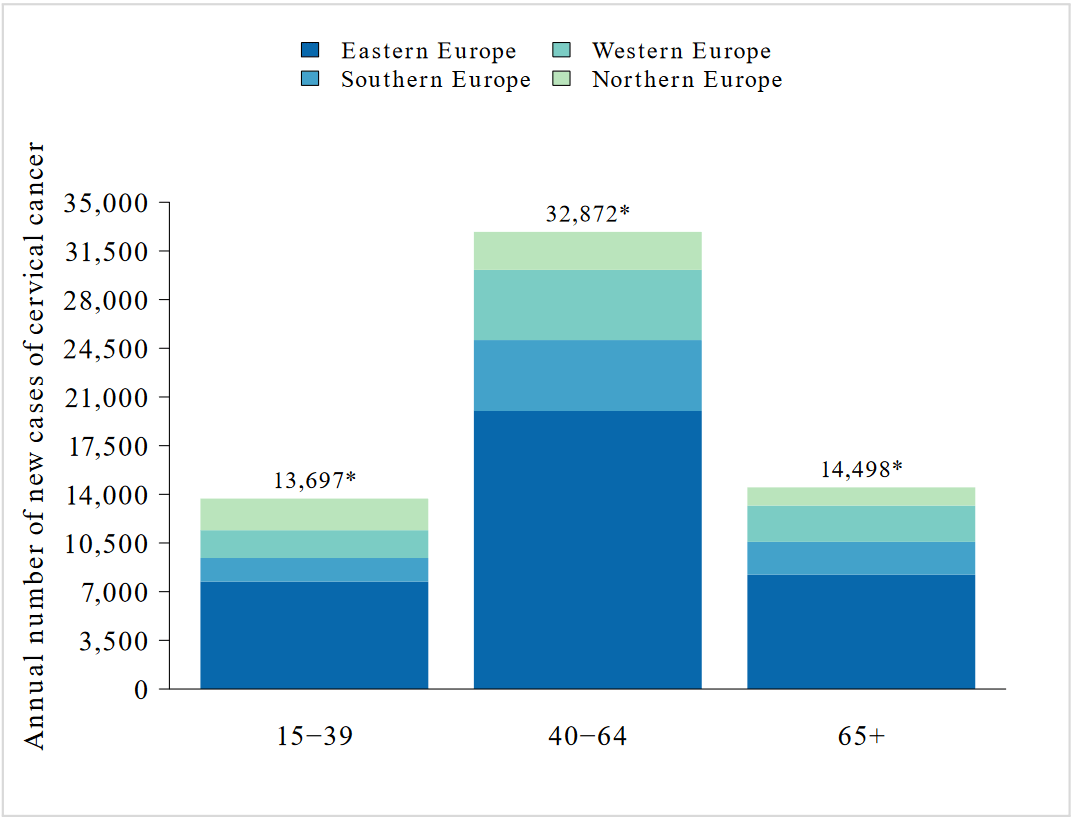
Annual number of new cases of cervical cancer by age group in European regions (Estimates for 2018)
*Eastern Europe 15-39 years: 7,721 cases. 40-64 years: 19,993 cases. 65+ years: 8,224 cases. *Southern Europe 15-39 years: 1,699 cases. 40-64 years: 5,100 cases. 65+ years: 2,355 cases. *Western Europe 15-39 years: 1,999 cases. 40-64 years: 5,043 cases. 65+ years: 2,614 cases. *Northern Europe 15-39 years: 2,278 cases. 40-64 years: 2,736 cases. 65+ years: 1,305 cases. Data retrieved: Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARCInformation Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and RelatedDiseases in Europe. Summary Report 17 June 2019
SIGNS AND SYMPTOMS
- The most common symptom is vaginal bleeding after intercourse
- Bleeding between periods
- Possible abnormal, vaginal discharge and discomfort
- Only one swollen leg
- Further back, leg or pelvic pain, fatigue, weight loss, or loss of appetite
In the early stages of the disease, there may be no obvious signs or symptoms that will tell a woman she is at risk. The only way to detect cancerous cells is by having a regular smear test every 2-3 years.
RISK FACTORS
- Genital infection with the human papilloma virus (HPV), some types can cause genital warts and can play a role in the development of cervical cancer. HPV is passed on during sexual intercourse with an infected partner. Condoms can decrease the risk of infection but not eliminate it. Areas which are not covered by a condom are still prone to infection.
- Sexual activity in early teens.
- Smoking.
- Possible long term use of oral contraceptives.
- Multiple sex partners for either woman or their partner.
PREVENTION
Having smear tests regularly. This will help identify changes in your cervical cells before these turn cancerous. Between 25 and 44 have a test every 3 years. Between 45 and 60 get tested at least every 5 years.
- Consider using condoms as a barrier method of contraception
- Cut down on smoking or better, give them up altogether.
- HPV Vaccination for girls between 9-14 years old. This is offered to all girls at second level school in their first year.
Women who have sex will usually have an HPV infection at some point in their lifetime. HPV vaccinations provide the greatest benefits for pre adolescents. Since women are most at risk to be infected and to develop cervical cancer from an infection, many countries only suggest vaccination for girls. Risk groups who include, men having sex with men, and individuals with an immune disease such as HIV are also recommended to be vaccinated.
DIAGNOSIS
If your medical expert feels that your symptoms require an investigation then they will arrange more testing for you. The tests help diagnose cervical cancer and they include:
Physical Examination:
The medical proactitioner or nurse will use a spculum, a medical instrument that creates a better view for examination purposes, to examine your cervix.
Colposcopy:
When examining your cervix, the medical practitioner will use a colposcope together with a bright light. This allows the magnification of the colposcope to improve theri view of the surface of your cervix.
Biopsy: The medcial expert will take a tissue sample from your cervix for further examination under a microscope to ensure they are not abnormal.
TREATMENT
- Early cancer (or pre cancer) can be treated with laser treatment. This can cure the cancer, without damaging the womb.
- Sometimes treatment may involve surgical removal of the cervix and the surrounding tissue, but by leaving the ovaries intact it leaves the woman able to have children.
THE CERVICAL SMEAR TEST / PAP SMEAR TEST
The cervical smear test is a simple test which shows if there are any changes in the cells of the cervix which could develop into cancer. To take the sample a special instrument called a speculum is inserted into the vagina. This helps open the vagina so a sample can be taken. The doctor will collect a sample of cells from your cervix with a small brush or a tiny wooden spatula. This sample is placed on a slide and sent off to the laboratory to be thoroughly checked. The results are given to your doctor. Cervical cancer is not life-threatening if it is caught early. Therefore, regular cervical smears are so important. Remember, most women with an abnormal smear test result do not have cancer of the cervix. Screening rates differ drastically between the European countries. In Latvia and Romania only 25% of women where tested, whereas in Austria or Sweden more than 80% of women had been screened regularly for cervical cancer between 2006 and 2016.
WHO SHOULD HAVE THIS TEST?
All women who are or have been sexually active should have a cervical smear test at least once every three years. The disease can take up to ten years untill it has developed.
WHERE CAN I HAVE A CERVICAL SMEAR TEST?
The test is available from family doctors, maternity hospitals, family planning and well woman centres. These are known as screening when nocancerous activity is found and should be taken regularly to help identify any changes. It involves putting a speculum gently into your vagina and take a small sample of cells from the cervix (at the neck of the womb). These cells are then tested in a laboratory to check and identify if there are any changes occuring in them. In Ireland the national screening programme is called Cervical Check and is open for women aged between 25 and 60 years of age. You can use this link for more information and arranging an examination.
Updated Sept 2019 by Marleen Koetz. Aug 2023 MM
Remenber, A CERVICAL SMEAR TEST MAY SAVE YOUR LIFE !
![]()
Cancom Index | Previous | Next