|
|
POLICY • BRIEF
European Institute of Women’s Health
Ovarian cancer: A silent killer
|
Download as PDF | Download as .doc | ***
Revised, 25th July – 2021
Ovarian cancer: A silent killer
Ovarian cancer is cancer originating in the cells of the ovaries and fallopian tubes. Ovarian cancer is the “silent killer” of women throughout Europe resulting in more deaths than any other women’s reproductive cancer. Globally, nearly 250,000 women each year are diagnosed with ovarian cancer, resulting in 140,000 deaths. Ovarian cancer is the 7th most common cancer and 6th most common cause of cancer death for women globally. In 2012, there were 65,000 cases of ovarian cancer in women in Europe. Annually, ovarian cancer results in more than 42,700 deaths in Europe. Europe has the highest rates of ovarian cancer in the world.1 2 3 4
Ovarian cancer symptoms can often be misattributed to other conditions, like gastrointestinal issues, and as a result, it is diagnosed at a late stage when it is difficult to treat. About 60% of those with ovarian cancer are diagnosed at a late stage (Stage III or IV) with significant implications for the success of treatment. Only 45% of women diagnosed with ovarian cancer survive for five years. Far too many women are dying from ovarian cancer each year. Despite its lethality, there are currently no effective population-based screening techniques for ovarian cancer nor simple test to diagnosis it. 5 6 7 The lack of sufficient screening and early detection results in substantive costs both for the patient herself and for the healthcare system as a whole. Stakeholders throughout Europe must work together to better combat ovarian cancer through increased awareness, improved diagnostics and comprehensive support.
Ovarian Cancer Rates Globally, 20128

Ovarian Cancer Risk Factors and Preventative Measures
Much about the development of ovarian cancer is not fully understood. Research must be urgently support to better understand the risk factors for ovarian cancer and to devise preventative measures that can be taken to combat this silent killer.
However, various factors are associated with the development of ovarian cancer. For example, in the United Kingdom, an estimated 21% of ovarian cancer cases are linked to lifestyle factors, including smoking, some types of hormone replacement therapy, and certain occupations.9 From 2002 to 2012, death rates from ovarian cancer decreased by 10% in the EU with significant cross-national variation across Member States with declines ranging from 0.6% to 28%. The reasons for the decline are not fully understood, though the increased use of oral contraception is believed to be a driving factor.10
Age
The risk of ovarian cancer increases with age. Most ovarian cancer develops in women after menopause, with over half of ovarian cancer cases occurring in women over the age of sixty-three. The highest rates of ovarian cancer occur in women ages 55-64. While ovarian cancer is rare in women below the age of forty, women experiencing the symptoms of ovarian cancer (such as bloating, changes in appetite, abdominal pain, or needing to urinate more often) should still speak to their doctor.11 12
Genetics
“An estimated 5-10% to 20-25% of ovarian cancer result from a genetic predisposition, depending on the country and study. 13 14“
The BRCA1 and BRCA2 genes account for 10-15% of ovarian cancer cases. These genes are linked to a high risk of cancer of the ovaries, breast, fallopian tube, and peritoneum. The risk is also elevated for pancreatic cancer and prostate cancer. This gene makes the cancer-preventing protein less effective. Up to 40% of women with the BRCA gene develop ovarian cancer. The risk of developing ovarian cancer over their lifetime is 35-70% in women with a BRCA1 mutation 10% and 30% in women with BRCA2 mutations. The risk of developing ovarian cancer is 1.4% in the general population. Women of Ashkenazi Jewish descent and Eastern European women have elevated risk of BRCA1 and BRCA2 mutations. 15 16 17 Those with BRCA mutations are often encouraged to have their ovaries and fallopian tubes removed by the time they reach the age of 40 to reduce the risk, which has repercussions for family life. 18
For more information and a BRCA animated guide can be found at:
https://eurohealth.ie/cancom/english/genetic-link/
Women with Lynch Syndrome (hereditary nonpolyposis colon cancer) have a 12% chance of developing ovarian cancer during their lifetime. Other syndromes that increase the risk for ovarian cancer development include PTEN tumor hamartoma syndrome (PHTS), Peutz-Jeghers syndrome and MUTYH-associated polyposis. 19 20
Ovarian cancer risk factors and preventative measures
Personal history of cancer and endometriosis
Women who have had breast cancer are at elevated risk of developing ovarian cancer, especially if they have BRCA1 or BRCA2 mutations. Women who had colon, uterine or rectum cancer also at increased risk of developing ovarian cancer. Endometriosis also increases the risk of developing certain types of ovarian cancer by two to three-fold. 21 22
Family history of cancer
Women whose mothers, sisters and/or daughters have ovarian cancer are at increased risk of developing ovarian cancer themselves. A family history of some types of colorectal, breast, uterine and rectal cancer is also linked to increased risk of developing ovarian cancer particularly if it linked to a genetic mutation.23
Reproductive and menstrual history
Women who have given birth prior to the age of 26 have a decreased risk of ovarian cancer. Those who have not had a child or first gave birth after the age of 35 are at elevated risk of developing ovarian cancer. Women who experienced infertility are also at increased risk of developing ovarian cancer. Breastfeeding may reduce the risk of developing ovarian cancer. 24, 25 Women who had early first menstruation (before the age of 12) or menopause after the age of 50 have increased risk of developing ovarian cancer.26 A hysterectomy (removing the uterus) can reduce the risk of ovarian cancer development by 1/3. Tubal ligation (having one’s tubes tied) can reduce the risk of ovarian cancer development by up to 2/3.27
Hormones
Women use oral contraception for 3-6 months or more are at reduced risk of developing ovarian cancer. The risk decreases with prolonged birth control use. The use of hormones after menopause has been linked to an elevated risk in developing ovarian cancer. 28, 29
Obesity
There is an increased risk of developing ovarian cancer in women who are obese (highly overweight; a body mass index exceeding 30). 30
Diet
Women who follow a low-fat diet have a decreased risk of developing ovarian cancer. Women who eat a large quantity of vegetables may also be at reduced risk of developing ovarian cancer.31
Ovarian cancer symptoms, diagnosis and screening
Many symptoms of ovarian cancer are not specific to ovarian cancer itself, which can delay diagnosis. Common symptoms of ovarian cancer include 32 33:
- Bloating: persistent bloating, increasing abdominal size
- Eating: trouble eating and quickly feeling full
- Pain: recurring pelvic and abdominal pain
- Urination: increase urination sensation and/or frequency
Other symptoms of ovarian cancer can include bowel changes, fatigue, unexplained weight loss and unusual bleeding.34, 35 Awareness amongst both women themselves and healthcare professionals on these symptoms must be increased.
Symptoms of ovarian cancer can often be misattributed to other medical condition like irritable bowel syndrome, which delays diagnosis of the cancer itself. Moreover, there is currently no population-based screening techniques available for ovarian cancer barring limited programming for women with BRCA mutations and a family inheritance. Various tests may be used for detecting ovarian cancer, including a blood test for a specific protein and scans, including CT scans and ultrasound. The final diagnosis involves a biopsy of the ovarian tissue.36, 37, 38
Ovarian cancer diagnosis is often delayed due to the lack of early screening and specific symptoms. About 60% of women are diagnosed at an advantaged stage (Stage III or IV). 39 Only about 25% of ovarian cancer diagnoses occur at Stage I. 40 The late diagnosis affects the treatment of the cancer, making it more difficult to effectively combat. Effective screening and early diagnosis techniques must be developed and systematically tested in order to tackle this lethal disease. 41
Some effective screening efforts have been developed for screening high risk women for ovarian cancer, those with a lifetime risk of 10% or more of developing ovarian cancer or those with two or more family members suffering from ovarian cancer.42, 43, 44. Initial evidence indicates that the ovarian cancer can be detected at an earlier stage for this population as they are at elevated risk.45, 46. It is unclear if early detection in high risk groups reduces the risk of death. 47. More evidence is needed, and best practice exchange should be encouraged and promoted to better screen for ovarian cancer, particularly for those at risk. Educational programmes and screening efforts should target those at risk, particularly those with BRCA mutations.
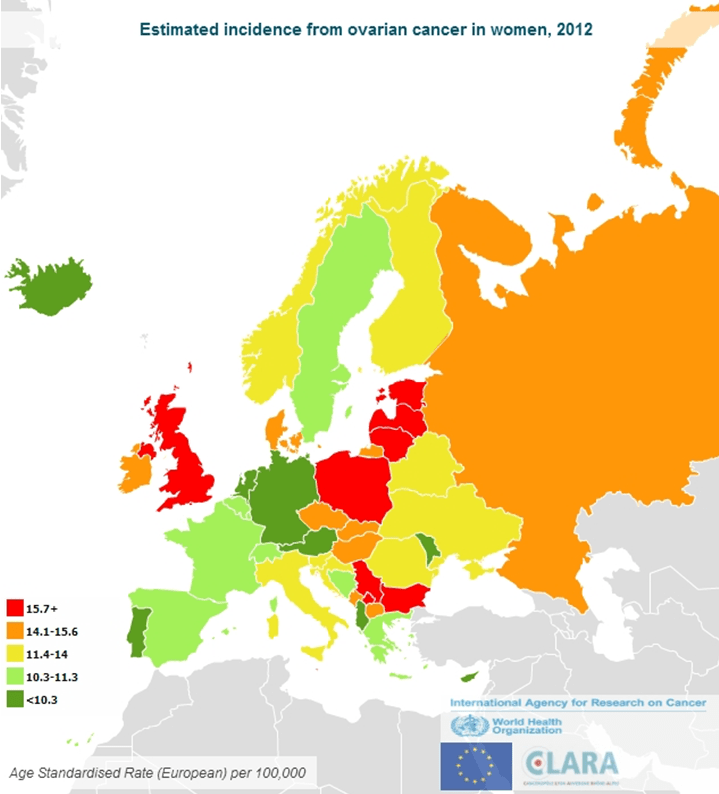
Ovarian Cancer Incidence, 2012 48
Ovarian cancer treatment and prognosis
Classifying ovarian cancer
The grade of cancer relates to how abnormal the cells appear when viewed under a microscope and provides some indication of how the cancer may behave. Stages describe the size of the cancer and whether or not it has spread to other parts of the body. The staging is used for treatment decisions. Stages indicate how much the cancer has grown and spread.49
There are four stages of ovarian cancer 50, 51
- Stage I: The cancer is only located in one or both of the ovaries.
- Stage II: The cancer has spread into the pelvis (hip bone) from the ovaries.
- Stage III: The cancer has moved outside the pelvis into the abdominal cavity.
- Stage IV: The cancer has spread to other distant organs in the body, like the lungs or liver.
The complete FIGO staging of cervical carcinomas is available online. 52
Ovarian cancer can be also be classified using the tumour, node, and metastasis (TNM) categorisation for cancer staging:
- Tumour (T): T describes the size of the tumour 53
- Node (N): N indicates whether (or not) and to what extent the tumour has spread to the lymph nodes 54
- Metastasis (M): M specifies whether or not the tumour has spread to other areas of the body, such as the liver or lungs.55,56.
Ovarian Cancer Mortality, 2012 57

Ovarian cancer treatment and prognosis
Treating and living with ovarian cancer
The treatment for ovarian cancer depends on its type, grade, location, spread, patient health and patient’s preference. Treatment options generally include surgery, chemotherapy and antibodies, with most women requiring surgery. Radiation therapy and/or hormone therapy may also be required. In addition, new targeted treatments have been developed to tackle BRCA mutated ovarian cancer by identifying and attacking cancer cells. BRCA testing is often recommended for ovarian cancer patients to improve treatment as well as prevention of other BRCA-related cancers.58. Treatment plans are tailored for each diagnosed patient.59, 60, 61. Personalised treatment plans should be supported, designed to meet individual needs.
If the ovarian cancer is caught early, some women may only require surgery. However, most ovarian cancer is diagnosed at a late stage. 62, 63 After initial treatment, 70% of those with Stages III-IV ovarian cancer relapse (i.e. if the cancer regrows). Treatments should be supported that limit relapse. Thus, improved treatment techniques must be supported, explored and developed in order to minimise the debilitating impact of ovarian cancer treatment on women’s daily lives.64
As previously discussed, due to a lack of screening options and early diagnostic techniques, 60% of women with ovarian cancer are diagnosed at the advanced stages (III and IV) 65. As a result, despite medical advances over the years, the five-year survival rate for ovarian cancer is 46%, which is largely due to its late stage diagnosis. Ovarian cancer has the highest mortality of all gynaecological cancers. 66 Only about a quarter of women diagnosed with ovarian cancer survive more than five years, and the ovarian cancer has an overall mortality rate of 75%.67 However, the five-year survival rate could be 90% if ovarian cancer was diagnosed at an early stage.68, 69 Ovarian cancer is killing far too many women in Europe annually and must be better tackled by improved screening and treatments.
The side effects of ovarian cancer treatment depend on the course and type of treatment. Various treatments may impact individual patients differently. However, patients can experience difficulty managing and coping with the treatments for ovarian cancer, particularly when it is treated at a later stage, which has physical, emotional and psychological implications. Chemotherapy can result in a range of side effects including but not limited to reduced appetite; constipation; nausea; vomiting; diarrhea; mouth and lip sores; alopecia; and polyneuropathy.70 Surgery has various implications, including its impact on fertility. New targeted therapies offer potential by treating specific targets, but they can also have substantive side effects like diarrhea and liver problems.71 Patients with ovarian cancer must be supported in order to best manage their condition and its treatment to lessen its day to day impact.
Overall, treatment for ovarian cancer is difficult on the patient. About 90% of women with ovarian cancer have fatigue during their treatment with implications for the quality of their life. 72 The majority of patients with ovarian cancer (over 70%) report suffering from sleep disturbances with many developing insomnia.73
Ovarian cancer treatment and prognosis
Mental health and ovarian cancer
Women diagnosed with ovarian cancer often face a poor prognosis and difficult treatment courses. Half of women with ovarian cancer have psychological distress. 74 Ovarian cancer increases the risk of depression in women throughout their treatment. Women who have ovarian cancer have higher rates of depression than women in the general population. Depression, particularly at an early stage of treatment, can negatively impact treatment plans and subsequently, survival.75, 76 Anxiety has also been found to be particularly elevated in women with ovarian cancer, especially prior to surgery. The anxiety rates are in fact typically higher than the rates of depression, particularly after treatment. 77 Some initial studies also suggest that there may be a link between depression and the development of ovarian cancer, which warrants further exploration.78 It is vital to holistically support those battling ovarian cancer and help them better manage their cancer and its side effects.
Despite the strong connection between mental health and ovarian cancer, women’s mental health can often be overlooked during diagnosis, treatment and recovery. Moreover, mental health can adversely influence the effectiveness of treatment.79 Concerted efforts must be made to diagnose, treat and support women with ovarian cancer not just for the cancer itself, but also for the psychological and emotional toll that it can take on women.
Inequities in ovarian cancer
Socio economic inequities are apparent in ovarian cancer from diagnosis through survival.80 For example, some studies suggest that women with lower educational attainment were more likely to be diagnosed with later stage ovarian cancer than those with higher education levels.81 This correlation warrants more investigation, particularly in a European context. Poorer and less educated women should receive the same treatment, care and prognosis as more affluent, educated women.
Evidence also suggests that there are racial influences in ovarian cancer diagnosis, treatment and survivorship. Findings from the United States also suggest that African American women have higher mortality and lower survival than white and Hispanic women.82 Other factors, like geographic location particularly with regard healthcare services, also appear to play a role. 83 Thus, inequities are evident from ovarian cancer prevention through treatment and survivorship, though much of the evidence is from American studies. There is a lack of information on ovarian cancer inequities in Europe, which urgently needs to be explored in order to combat these inequities.
Ovarian cancer treatment and prognosis
Employment, financial issues and ovarian cancer
Whether or not a woman with ovarian cancer is able to continue to work depends on the type of cancer, the treatment, the type of work and the patient’s overall health. Various treatments can have different impacts on the individual patient. However, most women will need to take some time off.84 Some women with cancer continue to work full-time during treatment. Others have to adjust their work arrangements depending on employer accommodation. Others are too tired or sick to work.85 Various studies explore the effect of cancer on employment. Few studies examine the impact of ovarian cancer specifically; this research must be supported and funded.
Most cancer patients face costs from their cancer diagnosis, treatment and recovery. These bills include medical, prescription, and travel costs. As patients are increasingly at home during treatment, utility bills may also rise. The extra costs of ovarian cancer combined with the decreased income from taking time off of work can result in financial difficulty for patients and their families. As a result, financial stress and strain may develop due to the cancer. Patients may have to take out loans, reduce other expenditures, or may fail to pay bills.86 The financial burden of cancer can cause “financial toxicity” for the patient and his/her family. This problem is particularly pronounced when the patient and/or their family members are unemployed or working in temporary (or part-time) positions during treatment and recovery.87 Ovarian cancer can be a particularly large challenge for single mothers. Programmes and policies need to be developed to support those with cancer during their treatment financially.
Cancer patients and cancer survivors can face discrimination from their employers. Consequently, women with ovarian cancer may make treatment decisions based on employment factors and fears of discrimination to the detriment to their health. This discrimination can be especially pronounced for women who are managers and entrepreneurs. Employers and policymakers should make efforts to reduce these barriers so that cancer patients and survivors are supported in the workplace through work adjustments during treatment and recovery. Some countries have rights to protect cancer patients from discrimination, though more support is required. Women with ovarian cancer should be supported and given options for their cancer management. Again, although there are many studies on other cancers, there is little evidence and data on this impact in women with ovarian cancer.88, 89 Additionally, programmes should be developed to empower working women with cancer.
In addition, most patients with ovarian cancer receive informal care from their families and/or close friends. This caring burden disproportionately falls on women and girls. Informal caregiving has large social, emotional, financial, and physical implications, but a lack of data regarding this phenomenon warrants further investigation in Europe. Caregiver support varies significantly throughout the EU,90 and there is a necessity for institutional recognition of the role. Thus, caregivers in addition to patients themselves need sufficient supports.
Ovarian cancer survivorship
Ovarian cancer has the lowest survival rate of all gynaecological cancers. There is wide variation across the EU with regard to survival rates, which is not fully understood.91
However, survival rates for ovarian cancer seem to drastically improve when patients are treated at specialised regional centres by gynaecological oncologists. The reason for increased survival rates is not fully understood but it is believed that the centres optimally utilise existing treatment and care practices.92 93 These centres should be funded and their development encouraged in countries in which they currently do not operate.
Ovarian cancer survivors receive regular follow-up, which includes medical appointments, imaging and blood tests. Cancer treatment plans can be helpful to many survivors. If the cancer either comes back or recurs, the patient will have to undergo treatment again. It is recommended that cancer survivors try to maintain a healthy lifestyle, which includes resting, eating well, staying active and minding their physical and mental health. 94 Women who had ovarian cancer should be supported in maintaining their overall physical and psychological well-being.
After treatment, elevated rates of psychological issues, physical symptoms (like pain), sexual problems and fear of recurrence can have a significant impact on survivors’ quality of life. Women should be supported and treated.95 Created in 2012, the European Network of Gynaecological Cancer Advocacy Group is a European patient advocacy groups network (ENGAGE) that supports and provides information to patients affected by gynaecological cancers.96 Support group and health literacy campaigns play a vital role in combating ovarian cancer.
Research, data and policy in Europe
Current state of European policy
The 2003 Council Recommendation on Cancer Screening calls on EU Member States to put breast, cervical, and colorectal cancer programmes in place for early detection of these cancers. Although the recommendation is not binding, it encourages Member States to develop effective population-based screening programmes.97 As there is no early detection or screening for ovarian cancer at the population level (only for high-risk individuals), ovarian cancer is not included in the guidelines.
However, the European Society for Medical Oncology (ESMO) has treatment guidelines for ovarian cancer that should be promoted, followed, monitored and improved.98 There is an opportunity to develop policy to prevent, diagnose and treat cancer as well as support patients both socially and economically. Efforts like the like the MEP Focus Group Dying to Work in the European Parliament and ESMO Patient Guide on Survivorship should be encouraged, promoted and expanded to support those currently living with cancer. Due to large variations in rates and trends in ovarian cancer across Europe, cross-national efforts to tackle this silent should be encouraged, including programmes for screening high-risk women.
Current state of European research
There are many gaps in the understanding of the development, progression, diagnosis, treatment and care of those with ovarian cancer. Must of the research has been conducted outside of Europe despite the elevated rates of ovarian cancer in Europe, and significant gaps in understanding continue to persist. The high mortality and lack of early detection of ovarian cancer must be urgently tackled through improved research in order to development better diagnostic techniques and care.
In Europe, there are ongoing efforts to increase research and improve treatment of ovarian cancer. The EU has funded various projects related to ovarian cancer, particularly with regard to research. These projects include but are not limited to the Horizon 2020-funded HERCULES, OCTIPS and PROCROP projects as well as the FP6-funded OVCAD project. In recent years, the European Medicines Agency has approved new targeted treatments for ovarian cancer. Orphan designation has been granted to some treatments of ovarian cancer by the European Medicines Agency.
Research, data and policy in Europe
Current state of European data
Cancer registries collect, manage, and analyse data on those with cancer in designated regions or in countries. The first cancer registry began in Hamburg, Germany in 1926. European-wide cancer registries began in the 1950s and 1960s. There are about 160 cancer registries in Europe at present covering about 72% of the population in the EU.99 The European Commission’s Europe Against Cancer Programme created the European Network of Cancer Registries (ENCR) in 1990 in order to foster collaboration between cancer registries, to train cancer registry personnel, to set standards for data collection, and to disseminate cancer data in Europe.100 With funding from the European Commission, the International Agency for Research on Cancer (IARC) in partnership with the ENCR developed the European Cancer Observatory (ECO), a system of information on the burden of cancer in Europe.101
Recently, the ENCR Secretariat moved to the European Commission’s Joint Research Centre, but no recent information on the ovarian cancer burden from the Europe-wide cancer registry data has been made available. 102 The most recent data from cancer registries, available on the ECO website, covers up to the 2007/2008 period. The GLOBOCAN Project has more recent ovarian cancer estimates, but these are estimates rather than register-based data from several countries, which do not provide reliable information on trends.103 EUROCARE publishes data on cancer survivorship based on information compiled from various registries. The WHO mortality database is a dominant source for information on ovarian cancer including data on ovarian cancer, yet it is not linked to the cancer registry, age, time or stage at the time of diagnosis. The mortality database only includes age and time of death from ovarian cancer not information with respect to the ovarian cancer diagnosis or progression. Thus, there is a lack of reliable, cross-national data that is sufficiently detailed on ovarian cancer.
The current registries collect a lot of information on ovarian cancer, including age, grade, and diagnosis date. However, there are limitations on the data available on ovarian cancer in Europe. Specifically, the data collected by cancer registries continues to vary by country. Moreover, much of the information collected is not compulsory. Additionally, not all countries track stage and treatment at diagnosis. Others do not have accurate survival calculations due to a lack of access to death certificates. In addition, not all capture information on survey, follow-up and co-morbidities. In various countries, the cancer registry is not linked to screening data. Thus, the standardisation and coverage of data must be improved. 104 Reliable cross-national data is essential to developing and implementing better policy, programming and practice to reduce the ovarian cancer burden in Europe.
Examples of national practice
Working together to combat the silent killer
Stakeholders must work at local, national and EU level to help combat ovarian cancer. Best practice should be exchanged in order to reduce inequities within and across European. Many organisations throughout Europe are working diligently to increase awareness of and support those with ovarian cancer.
Asociación de Afectados por Cáncer de Ovario (ASACO), Spain
ASACO was formed by women affected by ovarian and gynaecological cancers as well as by their relatives or caregivers, health professionals and other stakeholders who are involved in medical and psychological treatments. This is the first provincial-level association in Spain that specifically groups patients and close friends of oncological disease. ASACO operates support groups in Barcelona, Cantabria, Córdoba and Valencia informing, supporting and accompanying patients, families and caregivers. ASACO also produces health literacy information, including booklets and infographics on ovarian cancer.105
Deutsche Stiftung Eierstockkrebs, Germany
The German Ovarian Cancer Foundation has striven to inform patients and their relatives about the disease, advance research and support those with ovarian cancer. Annually, about 8,000 women in Germany are diagnosed with ovarian cancer. The quality of the treatment influences on the prognosis of the disease. The German Ovarian Cancer Foundation works to inform patients, families and healthcare professionals about this disease. They produce videos such as those on dealing with diagnosis of ovarian cancer, the BRCA gene mutation and new therapeutic available therapeutic approaches. They have also published a documentary about illness, therapy and living with ovarian cancer in German, Arabic, Turkish and English.106
STEPS FOR ACTION
- The EU and Member States must work together to improve policy and programmes to more forcefully tackle ovarian cancer.
Europe has disproportionately high rates of ovarian cancer from a global perspective. As the female population in Europe continues to age, ovarian cancer rates will rise in Europe. There is a lack of understanding about ovarian cancer, including recognising its symptoms. Health literacy campaigns to educate key stakeholders, including women themselves, about ovarian cancer should be promoted. These campaigns should include promotion of information on risk factors and symptoms of ovarian cancer as well as its links to other cancers, like breast cancer. Educational efforts should include awareness that genetic inheritance can occur from either patent, including the paternal side. More should be done to promote the understanding of ovarian cancer both amongst high risk groups and in the general population. Vulnerable groups should be specifically targeted, like those with the BRCA mutation.
- As there are currently no effective population-based screening programmes or early detection tests for ovarian cancer, efforts to better detect and screen for ovarian cancer should be researched, explored and supported urgently. Efforts to target women at high-risk of developing ovarian cancer must be supported.
Stakeholders across Europe and throughout the world must continue to promote the development and the improvement of ovarian cancer early detection and population-based screening efforts. The EU has undertaken many efforts to promote cooperation and harmonisation with regard to some cancer screening services and should encourage the development of early screening techniques for other forms of cancer like ovarian cancer. As part of effective national cancer plans, comprehensive national cancer registries should be supported to allow for cross-national analysis over time in order to develop more effective strategies and programmes to combat ovarian cancer. Some programming has been put into place to target women, such as women with BRCA mutations, at high risk of developing ovarian cancer. These targeted programmes must be put into place to support women at high risk of developing ovarian cancer.
- Initiatives need to be developed to better understand and to support women with ovarian cancer, physically, emotionally, and socially.
Initiatives should be developed that account age, cultural differences, and other relevant factors. Women with ovarian cancer face many physical, psychological, and financial burdens, particularly given the frequently late stage of their diagnosis. Programmes must be put into place to support patients with ovarian cancer, particularly those women with advanced or terminal cancer. Women should be educated on their cancer and the treatment options available to them. In order to reduce health inequalities, Europe must also encourage and support improved education, research, prevention, testing, and treatment initiatives specifically for disadvantaged groups of women, their families, and their communities.
- Encourage and support the implementation of ovarian cancer treatment guidelines.
Efforts should be made to ensure that the European Society for Medical Oncology (ESMO) treatment guidelines for ovarian cancer are followed across Europe. In addition, ovarian cancer patients should be treated in specialised clinics and performed by gynaecological oncologists, when possible, as patients have better outcomes. In addition, the ESMO Patient Guide on Survivorship should be promoted and implemented to help support those who are living with ovarian cancer.
- Strategies must be developed to support and empower ovarian cancer survivors throughout their recovery.
Strategies must be developed to support ovarian cancer survivors throughout their recovery to ensure that their health is managed and monitored. Moreover, survivors must be supported in their everyday lives, for example, by providing necessary employment supports through policy and programming. It is also important to empower survivors to help manage their own health. Efforts should also be made to ensure that more women survive from ovarian cancer given its particularly high mortality rate.
- Targeted research must be conducted by age, race/ethnicity and type of ovarian cancer in order to increase the understanding of the development, prevention, diagnosis, progression, and treatment of ovarian cancer, in the European region and in an international context.
Efforts must be made to better understand the development, progression, treatment, and prevention of ovarian cancer by employing a life-course approach from young through older age in Europe. Research must not only explore the biological aspects of ovarian cancer, but must also explore the mental, social, and economic implications for those with the disease as well as for those who survive it. Research must be conducted to better understand the trends of ovarian cancer in a European context as there is a lack of European data and studies in comparison to other countries. The EU should continue to fund projects on ovarian cancer. The European Medicines Agency should promote improved treatment for ovarian cancer. Global best practice exchange should be encouraged in order to better tackle ovarian cancer. However, practices must be regionally tailored for culture and other factors.
- Efforts must be taken in order to reduce health inequities with regard to ovarian cancer within and across Member States.
The EU together with the Member States and key stakeholder, including health organisations, patient organisations, and other relevant stakeholders, must encourage and support improved education, research, prevention, screening, and treatment guidelines. Europe must also provide guidance and support in to order to reduce health inequalities across Member States. Research to better understand inequities in ovarian cancer must also be promoted.
- In order to improve existing practice and policy, ovarian cancer data must be disaggregated based on various factors, including age and cancer stage.
A robust, comparable monitoring system to track ovarian cancer across Member States should be set up at the EU level to enable a concerted, common approach. Existing data collection tracking new and existing ovarian cancer cases and respective deaths from ovarian cancer across the EU must be improved and harmonised. Comprehensive, longitudinal data is essential to improve efforts to combat ovarian cancer as well as to assure quality and equity in prevention, diagnosis, treatment, and care.
A special thank you to AstraZeneca for an unrestricted educational grant that supported the generation of the:
“Women and Ovarian Cancer in the EU” policy brief.
A warm thank you to our expert reviewers:
- Elisabeth Baugh, Chair of the of the World Ovarian Cancer Coalition and CEO of Ovarian Cancer Canada
- Roisin Foster, Chief Executive at Cancer Focus NI and Treasurer of the Board of the Association of European Cancer Leagues (ECL)
- Lydia Makaroff, Director of the European Cancer Patient Coalition (ECPC)
- Eva Schumacher-Wulf, Board Member of the World Ovarian Cancer Coalition and Chief Editor of Mamma Mia! Magazine in Germany
Authors: Kristin Semancik and Peggy Maguire, May 2018
© 2018 – 22 European Institute of Women’s Health, CLG
33 Pearse Street, Dublin 2, Ireland
Telephone: +353-1-671-5691
Email: info@eurohealth.ie
Website: https://www.eurohealth.ie
References:
[1] World Ovarian Cancer Day. 2018. What is ovarian cancer? http://ovariancancerday.org/what-is-ovarian-cancer/.
[2] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[3] World Ovarian Cancer Coalition. 2017. Ovarian Cancer.
http://worldovariancancercoalition.org/#cancer
[4] ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
[5] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[6] World Ovarian Cancer Coalition. 2017. Ovarian Cancer.
http://worldovariancancercoalition.org/#cancer
[7] ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
[8] Reid, B. M., Permuth, J. B., & Sellers, T. A. (2017). Epidemiology of ovarian cancer: a review. Cancer biology & medicine, 14(1), 9.
[9] Cancer Research UK. 2016. Ovarian cancer risk factors.
http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/ovarian-cancer/risk-factors#heading-Zero
[10] American Society of Clinical Oncology. 2016. Study Examines Global Trends in Ovarian Cancer Mortality Rates
http://www.ascopost.com/News/43907
[11] American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
[12] Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
[13] American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
[14] Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
[15] American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
[16] Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
[17] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[18] ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
19 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
20 Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
21 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
22 Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
23 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
24 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
25 Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
26 Ovarian Cancer Research Fund Alliance. 2019. Risk Factors. https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
27 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
28 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
29 Ovarian Cancer Research Fund Alliance. 2019. Risk Factors.
https://ocrfa.org/patients/about-ovarian-cancer/risk-factors/
30 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html
31 American Cancer Society. 2016. What Are the Risk Factors for Ovarian Cancer?
https://www.cancer.org/cancer/ovarian-cancer/causes-risks-prevention/risk-factors.html.
32 European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf.
33 World Ovarian Cancer Day. 2018. What is ovarian cancer?
http://ovariancancerday.org/what-is-ovarian-cancer/.
34 World Ovarian Cancer Day. 2018. What is ovarian cancer?
http://ovariancancerday.org/what-is-ovarian-cancer/
35 ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf.
36 European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
37 ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
38 Teneriello, M. G., & Park, R. C. (1995). Early detection of ovarian cancer. CA: a cancer journal for clinicians, 45(2), 71-87.
39 European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
40 Badgwell, D., & Bast Jr, R. C. (2007). Early detection of ovarian cancer. Disease markers, 23(5, 6), 397-410.
41 Teneriello, M. G., & Park, R. C. (1995). Early detection of ovarian cancer. CA: a cancer journal for clinicians, 45(2), 71-87.
42 Mourits, M. J., & de Bock, G. H. (2017). European/US Comparison and Contrasts in Ovarian Cancer Screening and Prevention in a High-Risk Population. In American Society of Clinical Oncology educational book. American Society of Clinical Oncology. Meeting (Vol. 37, pp. 124-127).
43 Rosenthal, A. N., Fraser, L. S., Philpott, S., Manchanda, R., Burnell, M., Badman, P., … & Evans, D. G. (2017). Evidence of Stage Shift in Women Diagnosed With Ovarian Cancer During Phase II of the United Kingdom Familial Ovarian Cancer Screening Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, 35(13), 1411-1420.
44 Cancer Research UK. 2016. Ovarian Cancer: Screening.
http://www.cancerresearchuk.org/about-cancer/ovarian-cancer/getting-diagnosed/screening.
[45] Mourits, M. J., & de Bock, G. H. (2017). European/US Comparison and Contrasts in Ovarian Cancer Screening and Prevention in a High-Risk Population. In American Society of Clinical Oncology educational book. American Society of Clinical Oncology. Meeting (Vol. 37, pp. 124-127).
[46] Rosenthal, A. N., Fraser, L. S., Philpott, S., Manchanda, R., Burnell, M., Badman, P., & Evans, D. G. (2017). Evidence of Stage Shift in Women Diagnosed With Ovarian Cancer During Phase II of the United Kingdom Familial Ovarian Cancer Screening Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology, 35(13), 1411-1420.
[47] Memorial Sloan Kettering Cancer Center. 2018. Ovarian Cancer Screening Guidelines.
[48] IARC. EURCAN Factsheets.
https://ecis.jrc.ec.europa.eu/EUCAN/CancerOne.aspx
[49] Cancer Research UK. 2016. About stages and grades.
http://www.cancerresearchuk.org/about-cancer/ovarian-cancer/stages-grades/about-stages-and-grades
[50] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[51] Cancer Research UK. 2016. Staging Ovarian Cancer.
http://www.cancerresearchuk.org/about-cancer/ovarian-cancer/stages-grades/stage-1
[52] International Agency for Research on Cancer. 2018. A practical manual on visual screening for cervical neoplasia: Appendix 1 / FIGO staging of Cervical carcinomas.
http://screening.iarc.fr/viaviliappendix1.php
[53] Cancer Research UK. 2017. TNM Staging.
http://www.cancerresearchuk.org/about-cancer/breast-cancer/stages-types-grades/tnm-staging
[54] Cancer Research UK. 2017. TNM Staging.
http://www.cancerresearchuk.org/about-cancer/breast-cancer/stages-types-grades/tnm-staging
[55] Cancer Research UK. 2017. TNM Staging.
http://www.cancerresearchuk.org/about-cancer/breast-cancer/stages-types-grades/tnm-staging
[56] Cancer Research UK. 2017. Number Stages of Breast Cancer.
http://www.cancerresearchuk.org/about-cancer/breast-cancer/stages-types-grades/number-stages
[57] IARC. EURCAN Factsheets.
https://ecis.jrc.ec.europa.eu/EUCAN/CancerOne.aspx
[58] Neff RT, Senter L, Salani R. BRCA mutation in ovarian cancer: testing, implications and treatment considerations. Therapeutic Advances in Medical Oncology. 2017;9(8):519-531. doi:10.1177/1758834017714993
[59] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[60] Ovarian Cancer Research UK. 2016. Treatment Decisions.
http://www.cancerresearchuk.org/about-cancer/ovarian-cancer/treatment/treatment-decisions
[61] American Cancer Society. 2018. Targeting Ovarian Cancer.
https://www.cancer.org/cancer/ovarian-cancer/treating.html
[62] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[63] Ovarian Cancer Research UK. 2016. Treatment Decisions.
http://www.cancerresearchuk.org/about-cancer/ovarian-cancer/treatment/treatment-decisions
[64] European Network of Gynaecological Cancer Advocacy Groups. 2018. Ovarian Cancer Factsheet.
https://engage.esgo.org/media/2017/08/ENGAGe_What_is_ovarian_cancer_en_FINAL-2018.pdf
[65] ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
[66] Kaban, A., & Tekin, B. Depression and Anxiety in Ovarian Cancer. Natl Cancer Inst Monogr, 32, 57-71.
[67] Teneriello, M. G., & Park, R. C. (1995). Early detection of ovarian cancer. CA: a cancer journal for clinicians, 45(2), 71-87.
[68] Ovarian Cancer Awareness Month. 2018. Facts and Figures.
[69] Badgwell, D., & Bast Jr, R. C. (2007). Early detection of ovarian cancer. Disease markers, 23(5, 6), 397-410.
[70] Ovarian Cancer Research Fund Alliance. 2016. Chemotherapy Side Effects.
https://ocrfa.org/patients/about-ovarian-cancer/treatment/chemotherapy-side-effects/
[71] National Cancer Institute. 2018. Targeted Cancer Therapies.
[72] Kaban, A., & Tekin, B. Depression and Anxiety in Ovarian Cancer. Natl Cancer Inst Monogr, 32, 57-71.
[73] Kaban, A., & Tekin, B. Depression and Anxiety in Ovarian Cancer. Natl Cancer Inst Monogr, 32, 57-71.
[74] Kaban, A., & Tekin, B. Depression and Anxiety in Ovarian Cancer. Natl Cancer Inst Monogr, 32, 57-71.
[75] Watts S, Prescott P, Mason J, et al Depression and anxiety in ovarian cancer: a systematic review and meta-analysis of prevalence rates BMJ Open 2015;5:e007618. doi: 10.1136/bmjopen-2015-007618
[76] Kaban, A., & Tekin, B. Depression and Anxiety in Ovarian Cancer. Natl Cancer Inst Monogr, 32, 57-71
[77] Mielcarek, P., Nowicka-Sauer, K., & Kozaka, J. (2016). Anxiety and depression in patients with advanced ovarian cancer: a prospective study. Journal of Psychosomatic Obstetrics & Gynecology, 37(2), 57-67.
[78] Huang, T., Poole, E. M., Okereke, O. I., Kubzansky, L. D., Eliassen, A. H., Sood, A. K., … Tworoger, S. S. (2015). Depression and Risk of Epithelial Ovarian Cancer: Results from Two Large Prospective Cohort Studies. Gynecologic Oncology, 139(3), 481–486. http://doi.org/10.1016/j.ygyno.2015.10.004
[79] Kaban, A., & Tekin, B. Depression and Anxiety in Ovarian Cancer. Natl Cancer Inst Monogr, 32, 57-71.
[80] Srivastava, S. K., Ahmad, A., Miree, O., Patel, G. K., Singh, S., Rocconi, R. P., & Singh, A. P. (2017). Racial health disparities in ovarian cancer: not just black and white. Journal of Ovarian Research, 10, 58.
http://doi.org/10.1186/s13048-017-0355-y
[81] Præstegaard et al. 2016. “The association between socioeconomic status and tumour stage at diagnosis of ovarian cancer: A pooled analysis of 18 case-control studies.” Cancer Epidemiology. Volume 41. pp.71-79.
https://doi.org/10.1016/j.canep.2016.01.012
[82] Chornokur, G., Amankwah, E. K., Schildkraut, J. M., & Phelan, C. M. (2013). Global ovarian cancer health disparities. Gynecologic Oncology, 129(1), 258–264.
http://doi.org/10.1016/j.ygyno.2012.12.016
[83] Chornokur, G., Amankwah, E. K., Schildkraut, J. M., & Phelan, C. M. (2013). Global ovarian cancer health disparities. Gynecologic Oncology, 129(1), 258–264.
[84] Target Ovarian Cancer. 2016. Work and Finance.
[85] American Cancer Society. 2017. Working During Cancer Treatment.
[86] National Cancer Registry/Irish Cancer Society, Linda Sharp and Aileen Timmons. 2010.The Financial Impact of a Cancer Diagnosis.
http://www.ncri.ie/sites/ncri/files/pubs/FinancialImpactofaCancerDiagnosis%28FullReport%29.pdf
[87] Zafar SY, Abernethy AP. Financial Toxicity, Part I: A New Name for a Growing Problem. Oncology (Williston Park, NY). 2013;27(2):80-149.
[88] Tiedtke C, de Rijk A, Dierckx de Casterlé B, Christiaens MR, Donceel P. Experiences and concerns about ‘returning to work’ for women breast cancer survivors: a literature review. Psychooncology. 2010 Jul;19(7):677-83. doi: 10.1002/pon.1633.
[89] Islam T, Dahlui M, Majid HA, et al. Factors associated with return to work of breast cancer survivors: a systematic review. BMC Public Health. 2014;14(Suppl 3):S8. doi:10.1186/1471-2458-14-S3-S8.
[90] Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal Caregiving for Cancer Patients. Cancer. 2013;119(0 11):10.1002/cncr.28057. doi:10.1002/cncr.28057.
[91] Oberaigner, W., Minicozzi, P., Bielska-Lasota, M., Allemani, C., De Angelis, R., Mangone, L., … & Eurocare Working Group. (2012). Survival for ovarian cancer in Europe: the across-country variation did not shrink in the past decade. Acta Oncologica, 51(4), 441-453.
[92] Rachel Pugh. 2016. “Specialist centres could boost ovarian cancer survival rates – study.” The Guardian.
[93] Vernooij, F., Heintz, P., Witteveen, E., & van der Graaf, Y. (2007). The outcomes of ovarian cancer treatment are better when provided by gynecologic oncologists and in specialized hospitals: a systematic review. Gynecologic oncology, 105(3), 801-812.
[94] ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
[95] Ahmed-Lecheheb, D., & Joly, F. (2016). Ovarian cancer survivors’ quality of life: a systematic review. Journal of Cancer Survivorship, 10(5), 789-801.
[96] ESMO. 2017. Ovarian Cancer: An ESMO Guide for Patients.
https://www.esmo.org/content/download/10097/201883/file/EN-Ovarian-Cancer-Guide-for-Patients.pdf
[97] Office Journal of the Europe Union. 2003. 2003 Council Recommendation on Cancer.
http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2003:327:0034:0038:EN:PDF
[98] European Society for Medical Oncology. 2016. Ovarian Cancer Treatment Recommendations.
[99] Harry Comber, Alexander Katalinic, Nadya Dimitrova (European Network of Cancer Registries). 2016. Cancer registries and breast cancer quality of care in Europe. European Network of Cancer Registries.
[100] The European Network of Cancer Registries. 2017. About Us: the European Network of Cancer Registries. .
[101] IARC. 2012. European Cancer Observatory.
[102] ENCR. ND. Contact Us.
[103] IARC. 2017. The GLOBOCAN Project.
http://globocan.iarc.fr/Default.aspx
[104] The European Network of Cancer Registries. 2017. About Us: the European Network of Cancer Registries.
[105] Asociación de Afectados por Cáncer de Ovario y Ginecológico. 2018.
[106] The German Ovarian Cancer Foundation. 2018.
