|
Policy • Brief European Institute of Women’s Health Women and Cardiovascular Disease |
Download as .doc | .pdf | .mp3
Women and Cardiovascular Disease
Cardiovascular Disease: The Basics
Traditionally regarded as a male disease, cardiovascular disease (CVD) is the number one killer of women worldwide. It also is a major cause of serious illness and disability, costly to healthcare systems and destroys women’s quality of life. In the EU, CVD remains the top cause of death for women in each of the 27 EU countries.
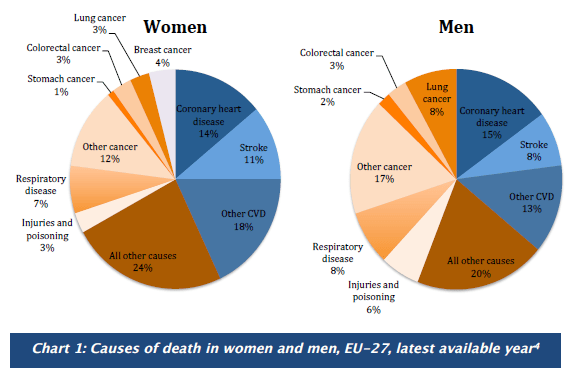
Only during the last decades has awareness been rising how CVD affects women differently from men, alerting women to their risk.Death from CVD accounted for 43% in women and 36% in men in the EU, see Chart. WHO defines cardiovascular diseases as a group of disorders of the heart and blood vessels that includes:
- Coronary heart disease (CHD): disease of blood vessels supplying the heart muscle.
- Cerebrovascular disease: disease of the blood vessels supplying the brain.
- Peripheral arterial disease: disease of blood vessels supplying the arms and legs.
- Rheumatic heart disease: damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria.
- Congenital heart disease: malformations of heart structure existing at birth.
- Deep vein thrombosis and pulmonary embolism: blood clots in the leg veins, which can dislodge and move to the heart and lungs
Heart attack and stroke are acute events, mainly caused by a blockage that prevents blood from flowing to the heart or brain.
Both can be life-threatening and may require immediate emergency treatment and hospitalisation. Time is of essence and influences survival chances. Coronary heart disease (CHD) by itself is the most common cause of death in the EU, responsible for more than 681,000 deaths annually; 14% of women and 15% of men die from CHD.
Women are much more likely to die within a year of having had a heart attack. Stroke is the second most common cause of death in women and affects more women than men. Although CVD has declined over the last 40 years, this decline has been smaller for women. Instead, new cases for women are rising and due to their greater longevity, the CVD burden can be said to have shifted gradually onto women.
CVD: Why Gender and Age Matters
The risk of CVD in women is still underestimated by society, including women themselves and the medici community. The reason for this is that CVD has been considered a male disease. Women are protected by their hormones against CVD during their fertile years, but lose this protection once they enter menopause.
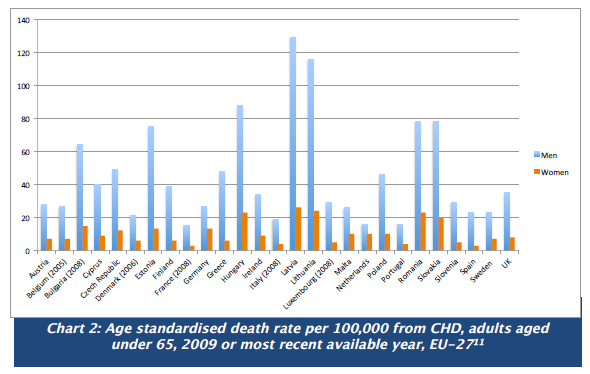
Women are getting CVD about 10 years later than men. Interlinked are other risk factors such as a rise in hypertension, which increases in women over the age of 45, as does total cholesterol level. Obesity, another major CVD risk factor, more prevalent in men under the age of 45, is increasing with advancing years in women. Thus, while younger women have a lower prevalence of CVD compared to men, this gap narrows and even reverses in older women. Across the EU, there are wide disparities in CVD.
Women experience different symptoms
To complicate matters, the symptoms of CVD in women can be different from those commonly observed in men, which may add to the under-recognition of heart disease in women. Women’s symptoms of a heart attack may be chest pain, but this can be less dramatic than in men.
Instead there may be an uncomfortable pressure in the centre of the chest which can last a few minutes, or come and go; pain or discomfort in one or both arms, the back, neck, jaw or stomach; shortness of breath with or without chest discomfort; or breaking out in a cold sweat, nausea or vomiting, light headedness or a general feeling of weakness. Women and thein doctors must be educated and trained to recognise the different symptoms. Women are slower to react when these symptoms strike, often losing valuable time in seeking emergency treatment.
Red Alert for Women’s Hearts
Although survival from CVD has improved over the last decades in men, women have yet to benefit. Several initiatives to raise awareness about CVD in women to improve prevention and treatment have been started by the major professional societies in the US and Europe. First off was the American Heart Association’s campaign entitled “Go Red for Women.
” Europe followed with “Red Alert for Women’s Hearts,” published by the European Society of Cardiology in 2009. These initiatives have raised the alarm bells about CVD in women. However, outside a few informed circles there is still a serious lack of awareness.
Strong communication messages are needed to address women themselves, explaining their risk factors and symptoms with the hope that such knowledge helps women to recognise their risk of heart disease and empowers them to change to a healthier lifestyle. It is estimated that 80% of CVD is due to lifestyle factors; therefore there is great opportunity for prevention.
Gender, Risk Factors, Hormones and CVD
Various risk factors for CVD manifest differently in women. Due to lack of awareness, women are less likely to understand and identify their risk factors, which makes CVD more difficult to prevent and manage. Age is an important factor for women who generally develop CVD ten years later than men.
During mid-life, more women than men develop hypertension and their total cholesterol level also increases. Both hypertension and elevated cholesterol are serious risk factors. Added to this is the increase of obesity in women over the age 45, which is characterised by body fat moving from around the hips up to the waist.
Although the age risk cannot be changed, other factors are amenable to prevention. During childbearing years, women seem to be protected from CVD by their hormones. After menopause a reduction in hormone levels is interlinked with a web of other risk factors such as central obesity, diabetes, hyperlipidemia, hypertension, history of smoking and metabolic syndrome.
The Controversy of Hormone Replacement (HRT)
The impact of HRT on cardiovascular disease has been a concern for women and their doctors for some time. In the past, it was recommended that medical professionals consider hormone replacement therapy (HRT) for use in post-menopausal women to limit CVD risk. In the meantime, randomised clinical trials have found mixed results of the risk/benefit of prescribing HRT to women for heart health. Doctors have become much more cautious and now recommend a careful evaluation of the risk/benefit before considering HRT replacement. Consequently, the use of HRT has declined.
Pregnancy and CVD
Heart disease is the leading cause of death during pregnancy. Fortunately, this is rare, affecting only an estimated 0.9% of pregnant women. To address the lack of understanding and guidance of heart disease in pregnancy, the European Society of Cardiology set up the first formal CVD pregnancy registry in 2007.
Findings from this registry reveal that pregnant women with a pre-existing heart disease have a 100-fold increased risk of death compared to pregnant women without heart disease. Reassuringly, results from the pregnancy registry show that most women with heart disease can go through pregnancy and delivery safely, as long as they are adequately evaluated, receive counselling and high quality care.
However to confound matters, many symptoms of heart disease – such as shortness of breath, fatigue and heartburn – are similar to general pregnancy symptoms, making heart disease during pregnancy difficult to recognise and diagnose. Women suffering from a congenital heart disease need to be careful as regards pregnancy and birth control options as both can increase heart risk in vulnerable populations.
The danger of smoking for CVD in women
Smoking is more likely to cause CVD in women than in men and research suggests that mortality in smoking women is higher. The risk of CVD is especially high in women who started smoking before the age of 15. It appears that women’s risk of CVD increases with the number of cigarettes smoked. As more and more young girls take up smoking, even out-smoking boys in some EU countries, every effort should be made to stop young girls and women from smoking.
General tobacco control messages have not been effective in reaching the target audience of young girls and women. Therefore, making messages and prevention programmes gender-sensitive as recommended by the WHO Framework Convention on Tobacco Control must urgently be instituted. Women appear to metabolise nicotine faster than men and get more easily addicted. The reasons are unclear and need to be better understood and studied.
Researchers at the University of Minnesota and Johns Hopkins University, when reviewing 30 years of research encompassing nearly four million people, found that women who smoked had a 25% higher risk of CVD than smoking men. For each additional year of smoking, a woman’s extra risk increased by 2%. Smoking resulted in an estimated 2.3 fold increased risk of heart attack compared to 1.8 fold risk in men. More research is needed to understand why women have an increased risk.
The underlying mechanism is unclear: is it biological, linked to hormones or related to differences in smoking behaviour, are women more vulnerable to passive smoking? Since on average women smoke fewer cigarettes than men, some research suggests that women who smoke might extract a greater quantity of carcinogens and other toxic substances from the same number of cigarettes.Women who smoke and take birth control pills, increase several times their risk of heart attack, stroke, blood clots, and peripheral vascular disease.
Under representation of women in clinical trials
Historically women have been under-represented in CVD clinical trials due to the mistaken belief that this disease mostly affects men. General clinical trial practice that considers one size-fits-all and fails to stratify trials’ results according to gender and age needs to be revised to include a robust risk/benefit analysis for both sexes.
Women with CVD have had to face the double discrimination of sex and age. Cost may have been another consideration, as women’s hormonal fluctuations tend to complicate the pharmacokinetic and pharmacodynamic picture. Paradoxically, CVD in women appears to be greatly influenced by hormones, a factor that has been used to exclude them from clinical studies. Moreover, if women have been included in clinical trials, results were not powered nor rigorously analysed for gender differences.
Unless such a systematic analysis is made a legal requirement, the future looks bleak for women. CVD, the number one lady-killer, is a glaring example of the lack of evidence how medicines work in women. Even in the US, where it is a legal requirement that research funded by the taxpayer’s money must include women and minority groups in the research, this is not standard practice.
A recent study found that trials by the National Heart Lung and Blood Institute, attached to the National Institutes of Health (NIH), included as little as 38% women for the years 1965 and 1998 and 27% between 1997 and 2006. Furthermore, only 13 of 19 studies analysed the gender differences. Gender-based CVD research fares even worse in Europe.
The current representation of women in European cardiovascular research has been assessed in the EuroHeart project with the sorry result that the proportion of women enrolled varied between 27 and 41% although the fiale prevalence of clinical conditions under study in the general population was similar for both men and women. The European regulator, the European Medicines Agency, responsible for approving medicines in Europe, must make gender and age analysis a legal requirement for approval to ensure that women and older people get evidence-based medicines.
Women with diabetes are at higher risk of CVD
Women with diabetes have more than double the risk of a heart attack than non-diabetic women. Diabetes doubles the risk of a second heart attack in women but not in men. The complex interconnection between diabetes and CVD in women has to be more intensively studied.
Diabetic women have a higher risk than diabetic men of developing coronary artery disease or stroke. After having suffered a heart attack, women’s prognosis is often poor with more women dying after one year. A meta-analysis shows that women with gestational diabetes have an increased risk of developing diabetes type 2.
Women CVD and depression
An American survey of women with heart conditions found that 57% of women said that they suffered depression, anxiety or both, following a heart attack. Cardiologists are usually not trained in recognising mental health problems which can be responsible for women failing to adopt a healthier lifestyle and thereby preventing another heart attack. In the complex field of chronic diseases, treating each disease in isolation would seem to be one of the biggest challenges to overcome. Rethinking of policy, medical training and treatment will be required better to address the chronic disease burden for both women and men.
Stop health inequalities – Urgent need to improve prevention and treatment
The misguided assumption that findings from research studies conducted on men applies equally to women has underserved women far too long. Women and older people of both sexes have rightly been called ‘the understudied majority’. This has to stop. The one-size-fits-all approach for patients will not succeed in helping to reduce the chronic disease burden. The increasing life years gained by women need to be flanked by a rigorous approach aiming to increase healthy life years. Increasing healthy life years by 2 % is an important aspirational goal of the EU 2020 strategy. New evidence has to be generated to inform a more enlightened research and health policy for chronic diseases. First, research must produce the evidence that is currently lacking how prevention such as low-dose aspirin, early diagnosis, diagnostic methods, medical devices and procedures, medicines for cholesterol lowering and controlling hypertension, and medical care are applied to the treatment of heart disease in women.
Major medical societies need to ensure that the acquired knowledge is widely distributed in the form of prevention and treatment guidelines that are rigorously implemented and followed. General practitioners, who by the nature of their work are in close contact with their female patients, need to better understand the complexity of CVD and the interconnection with lifestyle factors and other chronic diseases, trained to recognise symptoms, improve diagnosis and treat their patients according to the latest scientific sex and gender knowledge and standards of care.
Policy makers, researchers, clinicians, regulators, medical schools all have a role in engaging in a concerted effort to reduce the burden of chronic diseases by taking a gendersensitive, multi- and interdisciplinary approach that spans across the lifespan of women and men. Women themselves need to understand that they are at risk of CVD.
Gender & CVD Facts
- CVD is the leading cause of death among women—it is most preventable.
- Each year more women die from CVD than men.
- Stroke is the greatest cause of death from CVD in women.
- CVD symptoms in women differ from those of men.
- Women develop CVD after menopause, around 10 years later than men.
- Death from CVD occurs primarily in older women.
- Almost half of all women 60+ have hypertension and increased cholesterol levels.
- Diabetic women have a greater risk of CVD than diabetic men.
- Smoking presents a greater risk of CVD in women than men.
- Although women have a higher life expectancy than men, this brings with it a greater burden of chronic diseases, physical disability and loss of independent living.
Steps for Policy Action
- Improve existing EU data collection on CVD. Currently CVD data collection at the EU remains limited. Annual data about incidence and prevalence should also include the interaction and influence of major risk factors, presence of other chronic diseases, disaggregated by gender and age in order to fully understand CVD trends.
- Examine the interaction between CVD, gender, age, and other chronic diseases in women. Large gender differences exist in the development and progression of CVD in women. As women live longer and the prevalence of chronic diseases such as diabetes increases, it is important to understand the role that gender, age, and the interaction with other chronic conditions contribute to the development of CVD to better prevent and manage the overall chronic disease burden in women.
- Include women in clinical trials to develop evidence-based prevention, medicines, diagnostic and medical devices for women. Women, especially older women who are at particular risk of CVD, need to begreater burden of chronic diseases, physical disability and loss of independent living.included in statistically relevant numbers in clinical trials to ensure the greater burden of chronic diseases, physical disability and loss of independent living.approved medicine and treatments work effectively in women.
- Make smoking cessation policy and programmes gender sensitive in order to effectively reach young girls and women to stop smoking, thereby eliminating a major risk for CVD in women. Rates of smoking among young women are on the rise across Europe, with grave consequences for their future health and well-being. Studies demonstrate the alarming impact that smoking has on women and CVD. Tobacco-control programmes should target women, particularly disadvantaged groups, and women in those countries where smoking among young women is increasing.
- Tackle Europe’s obesity crisis, by making women as family caregivers more health-literate about the role of diet and exercise in preventing CVD and other chronic diseases. The risk of CVD can be lowered through healthy lifestyle choices. An unhealthy diet, lack of exercise and obesity are strongly linked to CVD.
- Increase awareness of CVD risks and symptoms among women. CVD remains the top killer of women in Europe and is responsible for much illness. Increased awareness of risk factors and symptoms is needed in order to combat this major cause of morbidity, mortality and disability in later years.
- Improve training of medical professionals in how to prevent and treat CVD in women and establish prevention and treatment guidelines. Major medical societies need to ensure that the aquired knowledge is widely distributed in the form of prevention and treatment guidelines that are rigorously implemented and followed. General practicioners need to better understand the complexity of CVD and the interconnection with lifestyle factors and other chronic diseases, trained to recognise symptoms, improve diagnosis and treat their patients according to the latest scientific sex and gender knowledge and standards of care.
- Policy makers, researchers, clinicians, regulators must engage in a concerted effort to reduce the burden of chronic diseases by taking a gender-sensitive and multi- and interdisciplinary approach reaching across the lifespan of women and men. The Joint Action for Chronic diseases is an opportunity to consider sex and age factors in a comprehensive approach to tackle Europe’s chronic dinase burden. Consideration of women and older patients must be included in this initiative.
References
All references were checked as working at time of publication. We are not responsible for links broken by sites who have a policy of moving information after publication.
- WebMD. 2012. World Heart Day focuses on women and children.
- European Heart Network. 2012. European cardiovascular disease statistics 2012.
- World Health Organization, Europe. 2013. Definition of cardiovascular diseases.
- Harvard Medical School. 2013. Gender matters: Heart disease risk in women.
- European Heart Network. 2012. European cardiovascular disease statistics 2012.
- Stramba-Badiale M, Fox K M, Priori S G, Collins P, Daly C, Graham I, Jonsson B, Schenck-Gustafsson K, Tendera M. 2006. “Cardiovascular diseases in women: a statement from the policy conference of the European Society of Cardiology” Eur Heart J 27:994-1005.
- European Heart Health Strategy. 2009. Red Alert on Women’s Hearts.
- M, et al. 2006. “Cardiovasculardiseases in women.”
- EHN. 2012. European cardiovascular disease.European Heart Health Strategy. 2009. Red Alert.
- Hughes, Sue. 2012. “ Heart disease is lead cause of death in pregnancy.” the heart.org
- Roos-Hesselink JW, Ruys TPE, Stein JI, et al. 2012 “Outcome of pregnancy in patients with structural or ischaemic heart disease: Results of a registry of the European Society of Cardiology.” Eur Heart.
- Vigl M, Kaemmerer et al. 2010. “Contraception in Women With Congenital Heart Disease.” American Journal of Cardiology 106(9): 1317-1321.
- Graham I, Atar D, Borch-Johnsen K, Boysen G, et al. 2007. “European guidelines on cardiovascular dinase prevention in clinical practice: executive summary.
- Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts).” Eur J Cardiovasc Prev Rehabil. 14, Suppl2:E1-40.
- http://www.ncbi.nlm.nih.gov/pubmed/17726406
- WebMD. 2012. Smoking and Heart Disease.
- 20. Woodward M and R Huxley. 2011. “Cigarette smoking as a risk factor for coronary heart disease in women compared
21. WebMD. 2012. Smoking and Heart Disease.
- Fahrenbruch, Kim C. CE, Menon V. 2008. “Enrollment of women in National Heart, Lung, and Blood Institute-Funded cardiovascular controlled trials fails to meet current federal mandates for inclusion.” JACC. 52:672–673.
23, 24.Stramba-Badiale, Marco. 2010. “Women and research on cardio vascular diseases in Europe: a report from the European Heart HealthStrategy project Marco Stramba-Badiale.” European HeartJournal 31, 1677–1685
- Ryde´n L, Standl E, Bartnik M, Van den Berghe G, Betteridge J, de Boer MJ, Cosentino F, Jo¨nsson B, Laakso M, Malmberg K, Priori S, O¨ stergren J, Toumilehto J, Thrainsdottir I, Vanhorebeek I, Stramba- Badiale M, Lindgren P, Qiao Q, Task Force on Diabetes, Cardiovascular Diseases of the European Society of Cardiology; European Association for the Study of Diabetes (EASD). 2007. “Guidelines on diabetes, prediabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the ESC (ESC) and of the European Association for the Study of Diabetes (EASD).” Eur Heart J. 28:88–136.
- Bellamy L, Casas JP, Hingorani AD, Williams D. 2009. “Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis.” Lancet. 373: 1773–1779.
- Lichtman, Judith, J. Thomas Bigger Jr, James A. Blumenthal, Nancy Frasure-Smith, Peter G. Kaufmann, François Lespérance, Daniel B. Mark, David S. Sheps, C. Barr Taylor, Erika Sivarajan Froelicher. 2008. “AHA Science Advisory. Depression and Coronary Heart Disease.” Circulation. 118: 1768-1775.
Special thanks to our expert reviewer:
Marco Stramba-Badiale, MD, PhD Director, Department of Geriatrics and Cardiovascular Medicine IRCCS Istituto Auxologico Italiano, Milan Italy